Retinal Detachment
A retinal detachment occurs when the retina is pulled away from its normal position in the back of the eye. The retina is the light-sensitive layer of tissue that lines the inside of the eye and sends visual messages through the optic nerve to the brain. Retinal detachment can cause permanent vision loss if not treated in time.
What happen in Retinal Detachment ?
A retinal detachment is a medical emergency in which the retina, a thin layer of tissue at the back of the eye that receives oxygen and nutrients from a layer of blood vessels, pulls away. Your vision may experience flashes and floaters as a result of retinal detachment.
HOW DO I KNOW IF I HAVE RETINAL DETACHMENT?
Symptoms of Retinal Detachment, if you have Retinal Detachment you may observe

Flashes of light (photopsia)
mostly experienced in the temporal (outside away from the nose) part of vision

Floaters
black cobweb-like spots moving in front of eye

shadow image
A curtain like shadow coming in field of vision
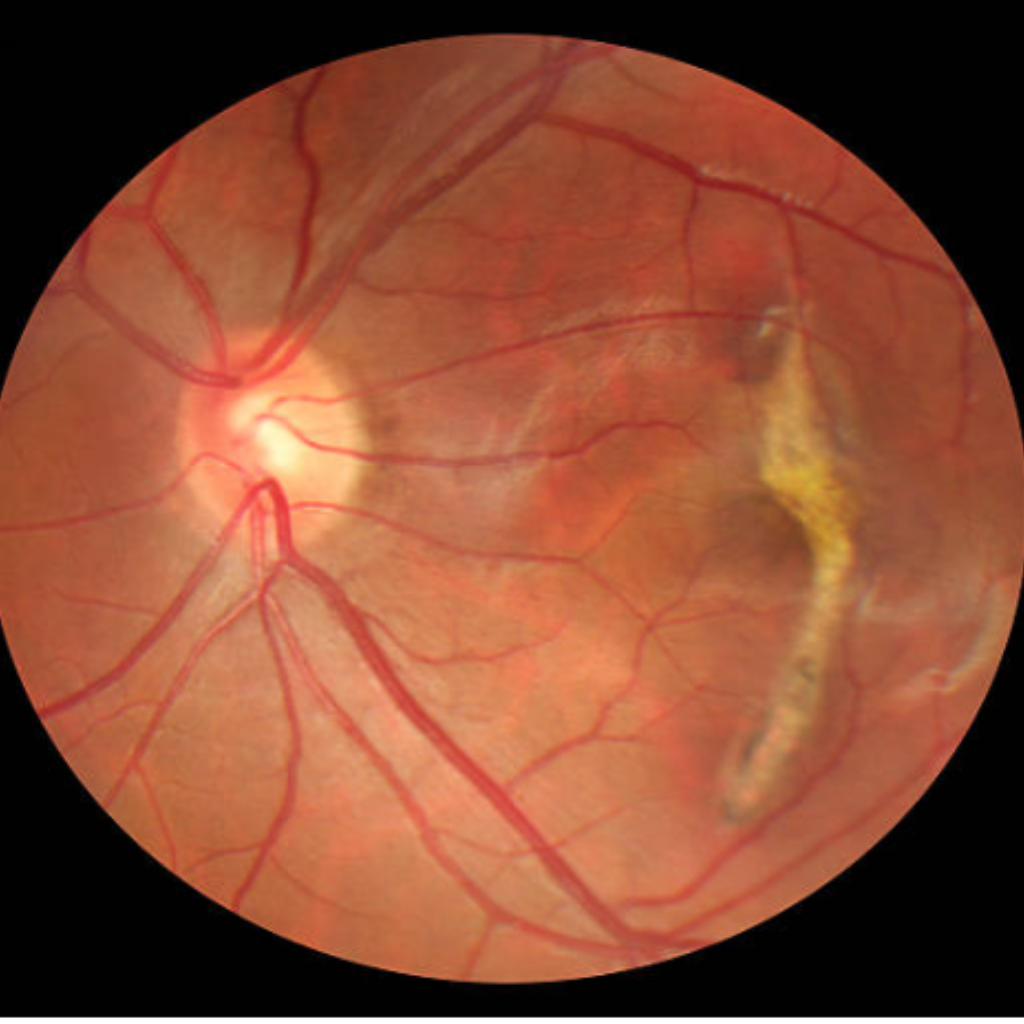
Detached Macula
Sudden Vision Loss when macula is detached
Medical Treatment for Retinal Detachment?
Retinal holes or breaks are treated with laser photocoagulation or cryopexy (a freeze treatment) as an outdoor procedure. During laser treatment, dot-like burns are placed around the hole to “weld” the retina. In Cryopexy the area around the hole is frozen and it helps reattach the retina. Retinal detachments are treated with surgery viz scleral buckling and complex vitreoretinal surgery involving the use of Silicon oil or gases.
In scleral bucking, a silicon band is placed and anchored with stitches around the eyeball to gently push the wall of the eye against the detached retina.
In vitrectomy – The surgeon makes tiny incisions in the sclera (white portion of the eye). Vitrectomy instruments are placed inside the eye to take out the vitreous gel and it is replaced with silicon oil or gases to push the retina in place. Laser or cryopexy is done around the brakes to seal it.
With modern vitreoretinal instrumentation, around 90 percent of cases with a retinal detachment can be successfully treated, Visual results are good if the retinal detachment is repaired before the macula (the center region of the retina responsible for fine, detailed vision) detaches. Thus it is important to contact your retina surgeon in time when you notice any flashes or floaters or a curtain in your field of vision.
Frequently Asked Questions
Few commonly asked questions about Retinal Detachment, these question will help you to understand better about Retinal Detachment.
Who is at risk for retinal detachment?
A retinal detachment can occur at any age, but it is more common in people over the age of 40.
Common risk factors for developing RD are-
High Myopia –Especially more than 5 Diopter – After cataract surgery. Retinal detachment in the other eye.
- Family history of retinal detachment.
- Presence of other eye diseases such as retinoschisis, degenerative myopia, or lattice degeneration.
- Following an eye injury.
what are the three types of retinal detachment?
There are 3 types of RD:
- Rhegmatogenous retinal detachment – A rhegmatogenous retinal detachment occurs due to a hole or break in the retina that allows fluid to pass into the space between the retina and other layers of the eye.
- Exudative or secondary retinal detachment – An exudative retinal detachment occurs due to inflammation that results in fluid accumulating underneath the retina without the presence of a hole or
- Tractional retinal detachment – A traction retinal detachment occurs when fibrovascular tissue on the surface of the retina pulls the retina from the underlying tissues as seen in diabetic retinopathy.
When should we get advice for retinal detachment?
If you see any retinal detachment symptoms, visit your eye doctor or the emergency department as soon as possible. Early intervention can aid in preventing irreversible vision loss. Regularly getting thorough dilated eye exams is also crucial.


